About
Profile and Contact

- M.B.B.S. - SCB Medical College, Cuttack - 1994-1999
- D.P.M.(Psychiatry)- Central Institute of Psychiatry, Ranchi (Ranchi University, Jharkhand, India)- 2003-2005
- M.D. (Psychiatry) - Central Institute of Psychiatry, Ranchi (Ranchi University, Jharkhand, India - 2008-2010
- Addiction psychiatry
- Adult Psychiatry
- Child Psychiatry & Psychology
- Mood clinic
- Behavioral sciences
- Governor's Award for the Best Young Doctor in 2014
- Chief Minister's Award for the Best Medical Teacher on Teachers Day 2017
- Rajdhani Samman by Govt of Odisha on Bhubaneshwar foundation for a contribution towards making Bhubaneshwar the smartest Smart City in the field of Medical Science for my initiative in making educational institutes Addiction free in 2018.
- Mother Teressa Award for my contribution to the Medical and Social fields in 2016.
- Annie Besant Award for my contribution to the field of education.
- R B Davies Award recipient
- As Mentor of a Professional Football team that won the Super Cup in 2023
- President, IPS Odisha State Branch (2022 and continuing)
- Editor, Odisha Journal of Psychiatry (2015 and continuing)
- Co-CHAIRPERSON, IPS Task Force on LGBT
- EC Coordinator of LGBT Task Force
- Chairperson, Website committee of IPS, East Zone
- Member, WPA Subsection on Psychiatry and Human Sexuality Section
- Assistant Editor of the International Journal of Psychosexual Health
- Treasurer, IPS, ODISHA STATE BRANCH(2013-15)
- Member, Indian Association of Private Psychiatry
- Convener, CME-Subcommittee of IPS on Consultation-Liaison Psychiatry (2014-16)
- Executive Council Member, IPS East Zone (2013-2016)
- Reviewer, Indian Journal of Urology
- Life Fellow: Indian Association for Geriatric Mental Health (IAGMH), India.
- Chairperson of Mental Health Helplines and National Anti-suicide Helpline
- Wellness Mentor of Odisha Football Cup
- 1st Chairperson of Task Force on Sports and mental health
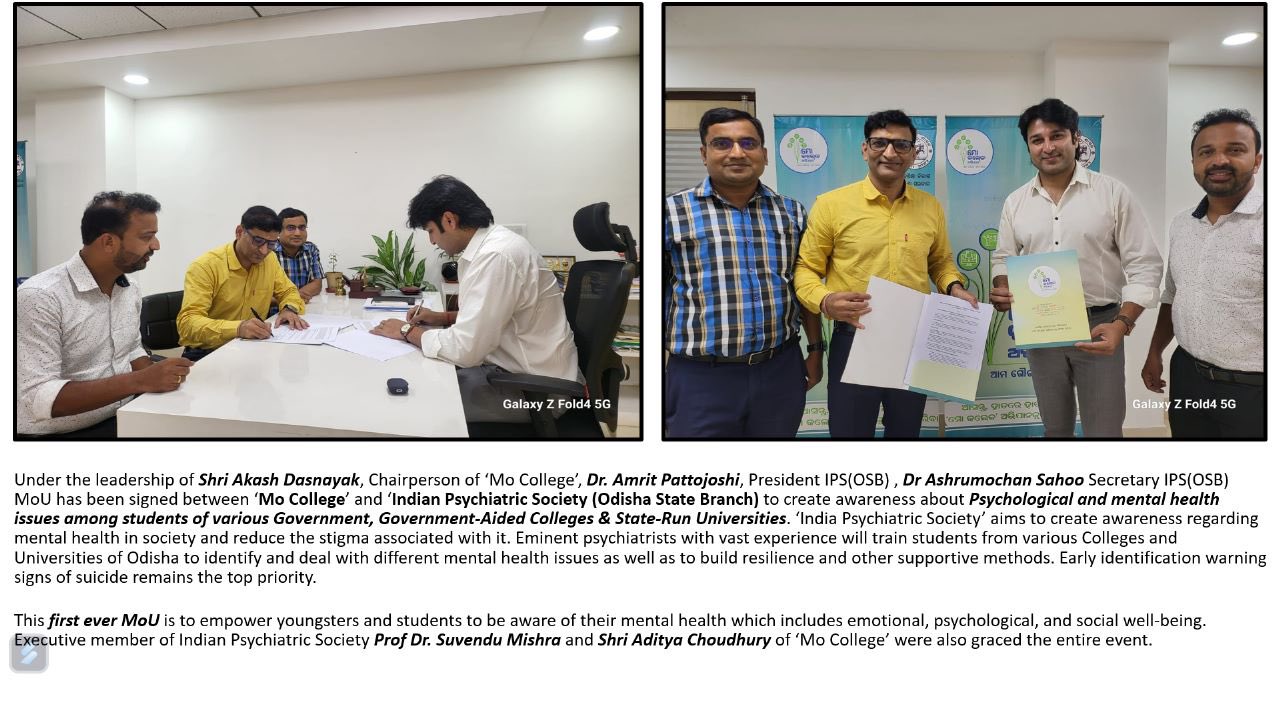
- As President of IPS, Odisha State Branch signed MoU with govt and Police dept for mental health services.
- Siddiqui, M. A., Pattojoshi, A. & Khess, C. R. (2016) Factors affecting adherence in patients with schizophrenia. International Journal of Advances in Medicine, 3 (1), 25-32.
- Siddiqui M A, Pattojoshi A, Munda S K, et al. (2015) Impact of psychopathology of adult obsessive compulsive disorder on quality of life: A patient controlled study. Journal of Evidence-Based Medicine and Healthcare; 2(56), 8865-71.
- Khan AH, Pattojoshi A, Siddiqui A, et al. Delusional drug dependence- an entity. J. Evolution Med. Dent. Sci. 2017;6(72):5172-5176, DOI: 10.14260/jemds/2017/1123
- Grover G, Avasthi A, Pattojoshi A, et al. [2015] Comorbidity in Patients with Dhat Syndrome: A Nationwide Multicentric Study. J of Sexual Medicine; 12[6] 1398-1401
- Lavania S; Ram D; Pattojoshi A, et al. (2012) Deliberate Self-harm in Nondepressed Substance-dependent Patients; Journal of Addiction Medicine, 6[4] 247?252
Services
Medication Management
Dr. Amrit Pattojoshi, a psychiatrist, provides meticulous medication management utilizing psychopharmacological interventions, conducting comprehensive assessments, prescribing appropriate medications, and monitoring treatment efficacy.
Psychotherapy
Dr. Amrit Pattojoshi, a psychiatrist, offers individualized psychotherapy sessions employing integrative modalities such as cognitive-behavioral therapy (CBT), psychodynamic therapy, and interpersonal therapy.
Diagnosis
Dr. Amrit Pattojoshi, a psychiatrist, provides meticulous psychiatric evaluations utilizing standardized diagnostic criteria and comprehensive medical histories to discern and categorize mental health disorders accurately.
Treatments
Drug Addiction
Dr. Amrit Pattojoshi, a psychiatrist, implements a comprehensive treatment plan involving pharmacotherapy, behavioral therapies, and relapse prevention strategies to address Substance Use Disorder, aiming to mitigate drug cravings, promote abstinence, and facilitate long-term recovery.
Sleep & Sexual Disorder
Dr. Amrit Pattojoshi, a psychiatrist, employs evidence-based interventions, including sleep hygiene techniques, cognitive-behavioral therapy (CBT), and pharmacotherapy, to address Sleep & Sexual Disorders, aiming to improve sleep quality and enhance sexual functioning.
Depression & Mood Disorder
Dr. Amrit Pattojoshi, a psychiatrist, employs a multimodal approach involving psychopharmacology and evidence-based psychotherapy to address Depression & Mood Disorders, aiming to restore neurochemical balance and enhance emotional well-being.
Schizophrenia
Dr. Amrit Pattojoshi, a psychiatrist, utilizes a comprehensive treatment regimen involving antipsychotic medications, cognitive remediation, and psychosocial interventions to manage Schizophrenia and optimize patients' psychopathological symptoms and functional outcomes.
Anxiety disorder
Dr. Amrit Pattojoshi, a psychiatrist, employs a multimodal therapeutic approach, combining anxiolytic medications, cognitive-behavioral therapy (CBT), and relaxation techniques to alleviate symptoms and enhance overall functioning in patients with Anxiety Disorders.
Dementia, Autism and ADHD
Dr. Amrit Pattojoshi, a psychiatrist, utilizes tailored treatment plans involving cognitive enhancers, behavioral interventions, and psychoeducation to manage Dementia, Autism Spectrum Disorder (ASD), and Attention-Deficit/Hyperactivity Disorder (ADHD).
For Online and Offline Consultation -
Gallery
- All
- Images
- Videos
Gallery
- Images
- Videos
Testimonials
Appointment
Contact
Location:
Plot no 14, reliance fresh, AG Colony, Unit 4, Bhouma Nagar, Bhubaneswar , Odisha, 751010
Email:
dramritp@yahoo.com
Call:
Not Available